For too long, both traditional PPOs and RBP models have protected insurer margins at the expense of employers and employees
- Auto-adjudicated claims mask hidden errors, duplicated charges, and fraud.
- 30% of employer healthcare spend is lost to waste and inefficiencies.
- Lack of transparency leaves you in the dark.
- RBP adds balance billing, legal risk, and member frustration on top of it all.
Bottom line: the healthcare system is broken — and employers are paying for it.
ProVision isn’t another add-on vendor. We’ve rebuilt the system from the ground up — blending PPO stability with audit-grade accountability.

20-25% total spend reduction

Keep your existing plan design

The nation's largest and most trusted PPO network

ACA-compliant, fully legal, and zero disruption

No balance billing. No hidden fees. No noise.

White-glove member experience

Performance Guarantee: If we don’t perform as promised, we don’t get paid.
We don’t promise savings — we prove them. Over 237,000 claims were processed and $211.9M in savings to our plan sponsors.
- Savings independently audited and validated
- More than 50% reduction in facility claims
- $0 balance billing issues reported
- 100% client retention since launch
- Every claim manually and AI-reviewed for accuracy
Slash spend without sacrificing care or coverage
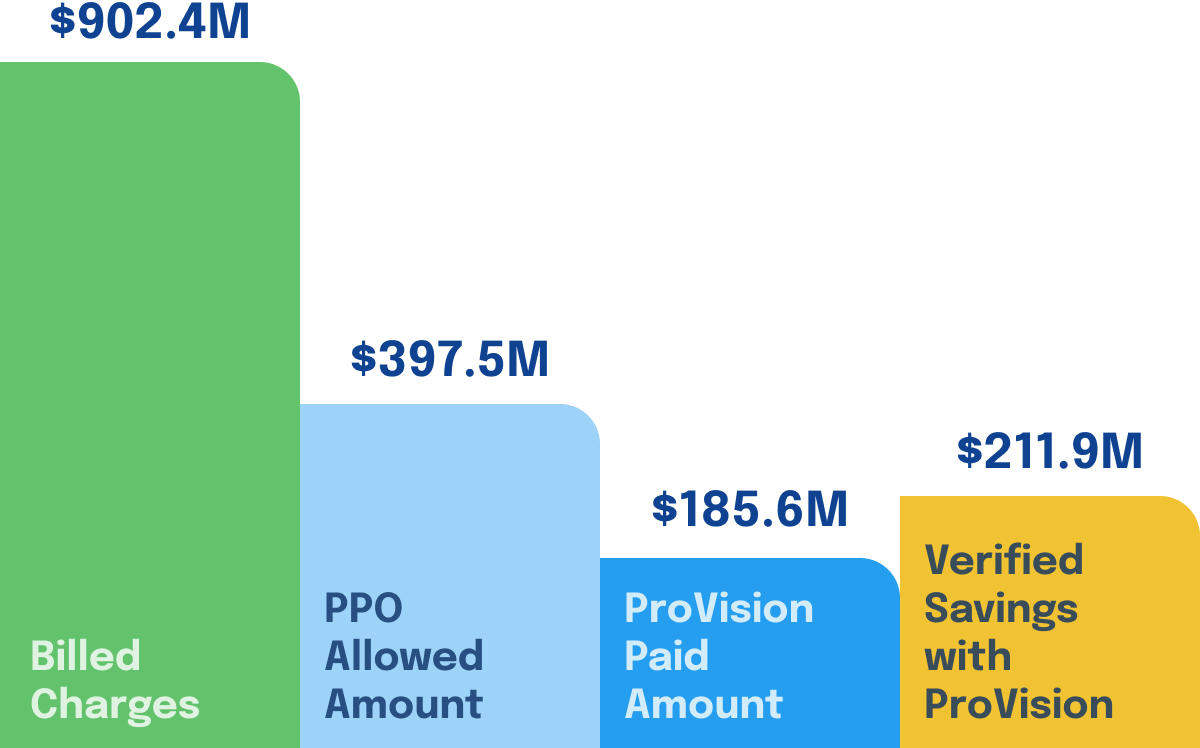
Data reflects performance from Jan 2022 to May 2025.

No disruption. No CapEx. Just EBITDA growth

Lower claims → lower premiums → stronger performance.

Nations largest and most trusted PPO network — zero member billing risk.

The only health plan in the US that offers a true and written performance guarantee.
- When we quote savings, we guarantee them. If we miss the mark on what we project, we will refund 100% of our sales fees. No hedging. No red tape.
- That's not typical in healthcare. That's ProVision Health.

No fluff. Just outcomes.
Let’s Explore What ProVision Could Do For You
